Patient Information
Patient Information
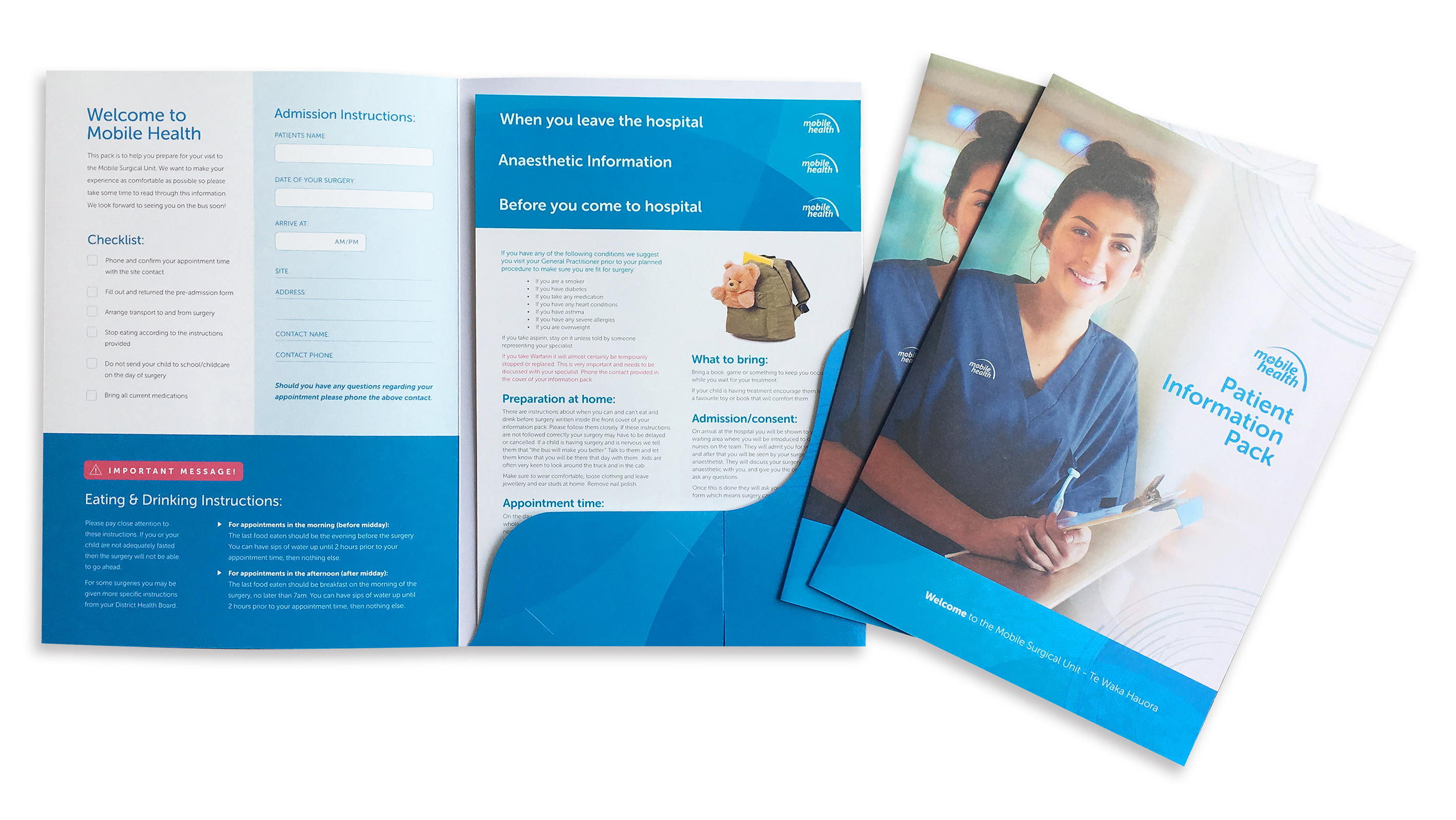
To help patients prepare for day surgery all patients will receive an information pack from their local Health New Zealand – Te Whatu Ora hospital. This pack will include information about preparing for surgery, what will happen on the day of surgery and information about going home after surgery.
Everybody’s circumstances are different, so if you have any questions or concerns please do not hesitate to ask questions at any stage. There will be a contact name and number inside this information pack for you to contact.
Mobile Surgical Unit
A mobile surgical unit is very unique, but once inside it is much like a standard operating theatre. The unit contains a modern and well-equipped theatre space which has been specifically designed and built for elective day surgery in rural areas. Additional information on the mobile surgical unit can be found here.

IMPORTANT: Eating and Drinking Instructions
You will find instructions on when you can and can’t eat and drink in your information pack.
Please pay close attention to these instructions. If you or your child are not adequately fasted then the surgery will not be able to go ahead. For some surgeries you may be given more specific instructions from your district health board.
Patient Information Pack
All patients will receive an information pack before surgery which should provide you with all the information you require to prepare for your procedure. This section includes a summary of the information you will receive, but please note your pack may include supplementary information specific to your operation.
To download the Patient Information Pack
You can also view the patient information below.
Day Surgery for Rural New Zealand
Learn more about the mobile surgical service, click here to view our service brochure.
Before you come for surgery
To view the before you come for surgery brochure click here.
On the day of surgery
To view the on the day of surgery brochure click here.
Anaesthetic information
To view the Anaesthetic information brochure click here.
After Surgery
To view the after surgery brochure click here.
Dental Surgery
To view the Understanding your childs dental treatment information click here.
Before you come to hospital
If you have any of the following conditions we suggest you visit your General Practitioner prior to your planned procedure to make sure you are fit for surgery:
- If you are a smoker
- If you have diabetes
- If you take any medication
- If you have any heart conditions
- If you have asthma
- If you have any severe allergies
- If you are overweight
If you take aspirin, stay on it unless told by someone representing your specialist.
If you take Warfarin it will almost certainly be temporarily stopped or replaced. This is very important and needs to be discussed with your specialist. Phone the contact provided in the cover of your information pack.
Preparation at home: There are instructions about when you can and can’t eat and drink before surgery written inside the front cover of your information pack. Please follow them closely. If these instructions are not followed correctly your surgery may have to be delayed or
Appointment time: On the day of your appointment, make sure that you keep the whole day free. The time in your admission pack is the time we need you to arrive at the hospital. You may have to wait for a while before surgery, but
Admission/consent: On arrival at the hospital you will be shown to your waiting area where you will be introduced to one of the nurses on the team. They will admit you for your surgery and after that you will be seen by your surgeon and anaesthetist. They will discuss your surgery and anaesthetic with you and give you the opportunity to ask any questions. Once this is done, they will ask you to sign the consent form which means surgery can then go ahead.
Operation: The bus staff will come and get you when it is time for your treatment. If you want a family member or friend to accompany you on board that is fine. Parents or guardians are allowed to accompany their child onboard, and one caregiver may stay with the child while they fall to sleep.
What to bring:
- Bring a book, game or something to keep you occupied while you wait for your treatment.
- If your child is having treatment encourage them to bring a favourite toy or book that will comfort them.
Anaesthetic information
Types of
- General
anaesthesia (GA) – Thisanaesthetic will put you to sleep for the whole operation. - Regional
anaesthesia – Theanaesthetist makes a region of your body numb so you won’t feel anything during your surgery, even though you may be awake. - Local
anaesthesia – Theanaesthetist will numb a small area where you will get treatment. - Monitored sedation – your
anaesthetist or surgeon uses a special range of drugs to keep you comfortable and sleepy but still able to respond to questions if needed.
What do I do before my anaesthetic? There are instructions about when you can and can’t eat and drink written inside the cover of your information pack. Please make sure that you follow them. It is very important that you have an empty stomach before your procedure. This means no eating or drinking before surgery.
Who is my anaesthetist? An anaesthetist is an experienced specialist doctor. They administer your anaesthetic, make sure you are safe during your operation and comfortable afterwards. Your anaesthetist will talk to you before the surgery and let you know everything that will happen that day. The anaesthetist looking after you is going to ask you some questions about your history so they can give you the best care. Anything that you tell the anaesthetist, the surgeon or the nurses will remain completely confidential. They will ask you about:
- Any history of drug allergies or problems with anaesthetics that you or your family may have had.
- Any illnesses or medical conditions in your family.
- Any illnesses that you have or medications that you are on.
If you regularly take medication or use an inhaler please bring them with you and show the
What will happen? Once your anaesthetist has spoken to you and you feel comfortable you will wait to be taken into the theatre on the bus. Your anaesthetist and the theatre team will help you lie down on the operating table while they connect you to the anaesthetic machine. There may seem to be a lot of people in theatre but everyone has a job to do and it is all about looking after you. You may also be asked to breathe through an oxygen mask while the anaesthetist gives you your anaesthetic.
Waking up You will wake up in our recovery area where one of our nurses will look after you and monitor you. When you feel well enough and are more comfortable we will give you sips of water and a cup of tea or coffee. You will stay in the day ward until you feel well enough to be discharged.
Remember: You must have a responsible adult to drive you home. You will not be permitted to drive after general anaesthetic or sedation.
When you leave hospital
When can I go home? After
Discharge information After surgery we will give you a copy of your operative record. Take this with you if you need to visit your GP. The nurse may give you some specialist post-operative instructions and will tell you if you need an appointment for follow up. We may also give you a prescription for medication to take after your surgery. It is important that you get this filled quickly and follow the instructions closely. If you are unable to get the medication please let the staff know.
The hospital or Te Whatu Ora – Health NZ may contact you the following day. A follow-up nurse from Mobile Health will contact you 30 days after your procedure.
Getting home after your operation Please ensure that you have arranged for someone to drive you
We recommend you have an adult stay with you for 24 hours after surgery.
Taking care after your operation Remember that if you have had a general
Surgery site Keep the dressing clean and dry. The amount of bleeding depends on the type of surgery that you have and a small amount of spotting on the dressing is normal. You may change the dressing if you were given spares after your surgery.
If the dressing becomes saturated and you have active bleeding seek medical assistance immediately, either GP or emergency care. Apply pressure until you get help.
Keeping the surgery site elevated will decrease swelling and discomfort.
Pain relief If the nurse has given you a prescription take this as directed for pain relief. Otherwise, use paracetamol (Panadol/Pamol) to control pain following the directions on the packet.
CONTACT YOUR DOCTOR IF ANY OF THE FOLLOWING OCCUR:
- Severe
pain, increased or excessive swelling. - Persistent discharge or excessive bleeding.
- Progressive heat and redness of the skin around the wound with increased pain and chills or fever.
- Difficulty moving.
- Pain, swelling or tenderness in calf or thigh.
Mobile Surgical Unit – patient experience
This short video shows the patient experience onboard the mobile surgical unit.
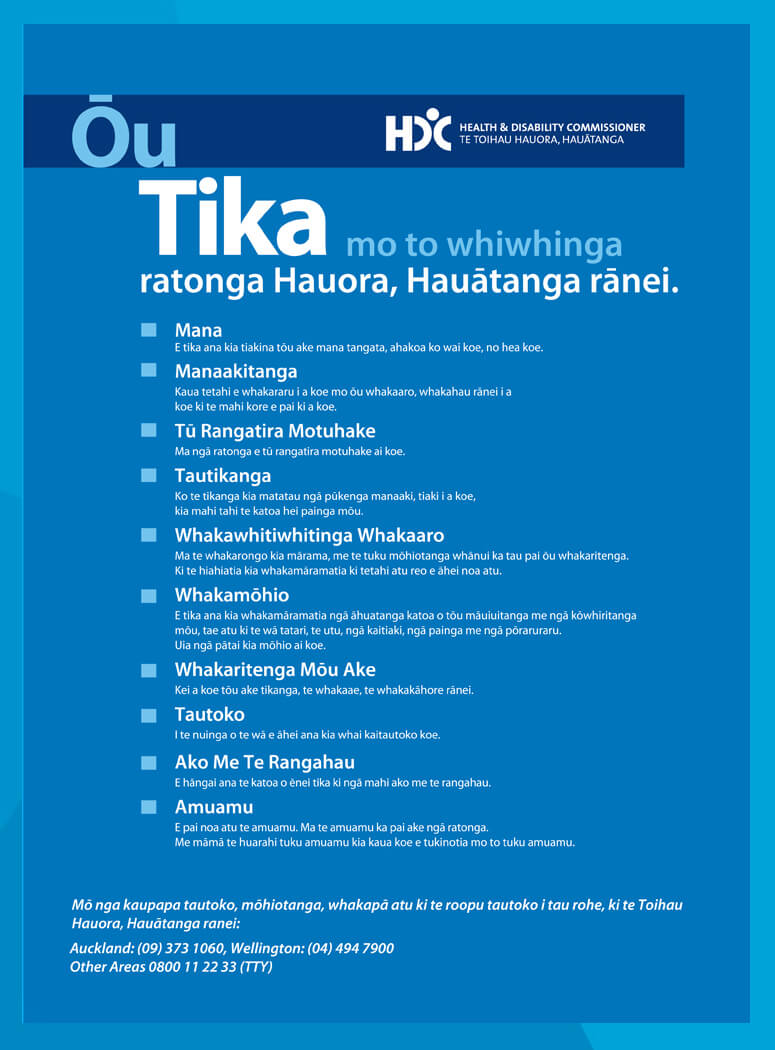
Your Rights
At all times we endeavour to meet your rights as outlined by the Health and Disability Commissioner. Please contact us if you feel we have not met your needs.
If you feel that we have not responded to your concerns, or if you would like independent and confidential advice or support, you can contact the Nationwide Health and Disability Commissioners Advocacy Service. Patient Advocacy Services can be contacted on 0800 555 050. Please refer to the attached brochure at the bottom of this page for information on this free and independent service.
At any time, you may access your own patient notes, to do this please contact us.
A minimal data set is held there, and you will be directed to the relevant district health board contact should further information be required.
© Mobile Health Group
Website by Qora Health Branding